DZ-Vent: Guide for making a low-cost mechanical ventilator for COVID-19 patients
Guide for making a low-cost mechanical ventilator
Prepared by Dr. Abdennour Abbas, University of Minnesota, USA
Purpose: This document provides information and resources to build a low-cost mechanical ventilator for COVID-19 patients when there is a shortage of automated medical ventilators.
Note: Any team composed of an electrical/mechanical engineer and an anesthesiologist can build this simple system.
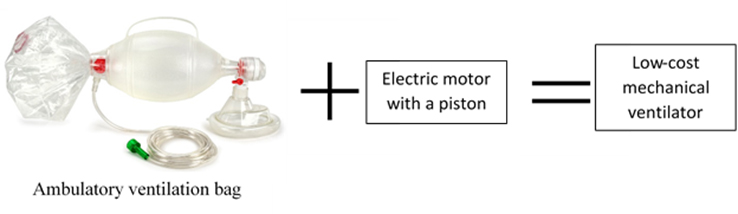
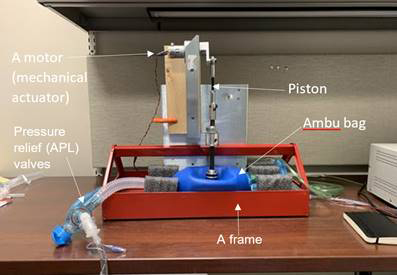
The mechanical low-cost ventilator is a “frame and mechanical actuator that will stabilize and compress a commercially available ambulatory ventilation bag connected to the patient’s endotracheal tube and external compressed oxygen, or if oxygen is not available, ambient air”.
Basically, it's a simple ambulatory ventilation bag or ambu bag (the bag that paramedic use to resuscitate patients in the ambulance manually squeezing with their hands), but instead of squeezing with the hands, a motor or a mechanical actuator will continually squeeze the bag. The most important piece is the mechanical actuator. The mechanical actuator is an electric motor that turns cranks that push a piston up and down and the piston pushes the ambu bag.
Expertise needed:
- Medical doctor (Anesthesiologist)
- Electrical and /or mechanical Engineer/ Bomedical engineer
- Production partner/manufacturer
Materials needed:
- A frame: The frame can be metal-stamped, 3D-printed or modified consumer goods.
- Ambulatory ventilation bag
- Pressure relief valves or APL (Adjustable pressure-limiting valve)
- Sheet metal fabrication (laser or water jet),
- Ball joint rod ends
- Mechanical actuator
-
A soirce of oxygen or if oxygen is not available, ambient air
- A 3-D printer is not required but could make things easy.
A Research article: "Design and Prototyping of a Low-cost Portable Mechanical Ventilator "
Read or download the the article here.
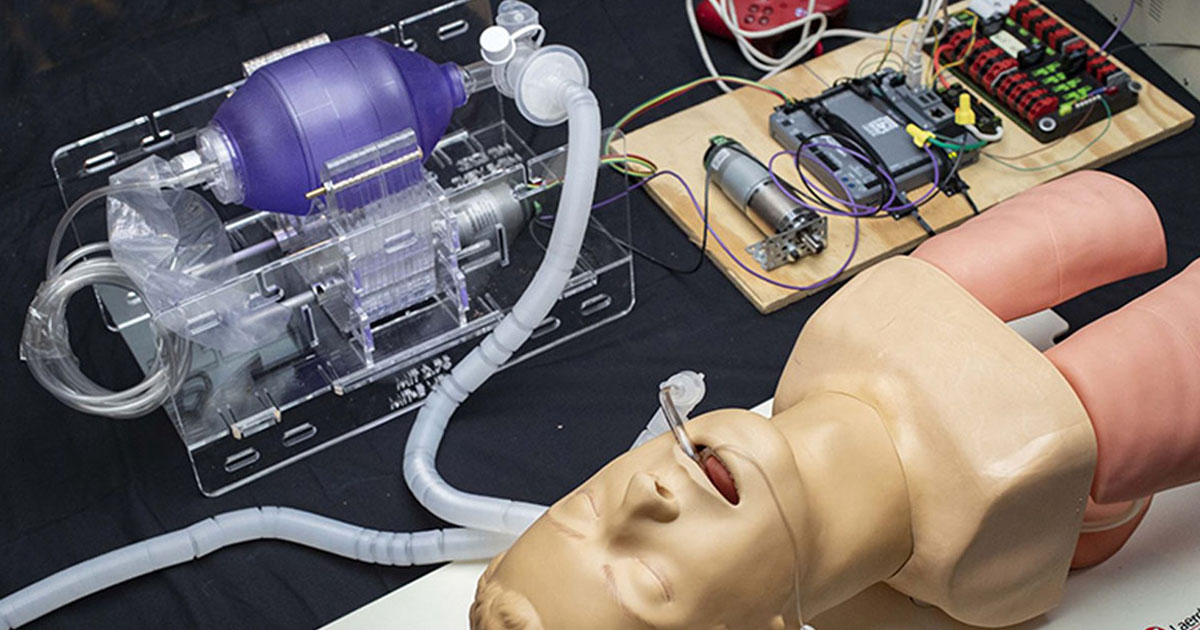
University of Minnesota Ventilator

OpenVent open source ventilator project - hackathon
OpenVent is an open source ventilator with an ambu bag (bag valve mask) plus maker components like stepper motors, 3D printed components, motor drivers, sensors, and Arduino,
For help with your design, send an email to: contact.openvent@gmail.com
For more information, please watch the video at: https://youtu.be/LgbF94eOf6w
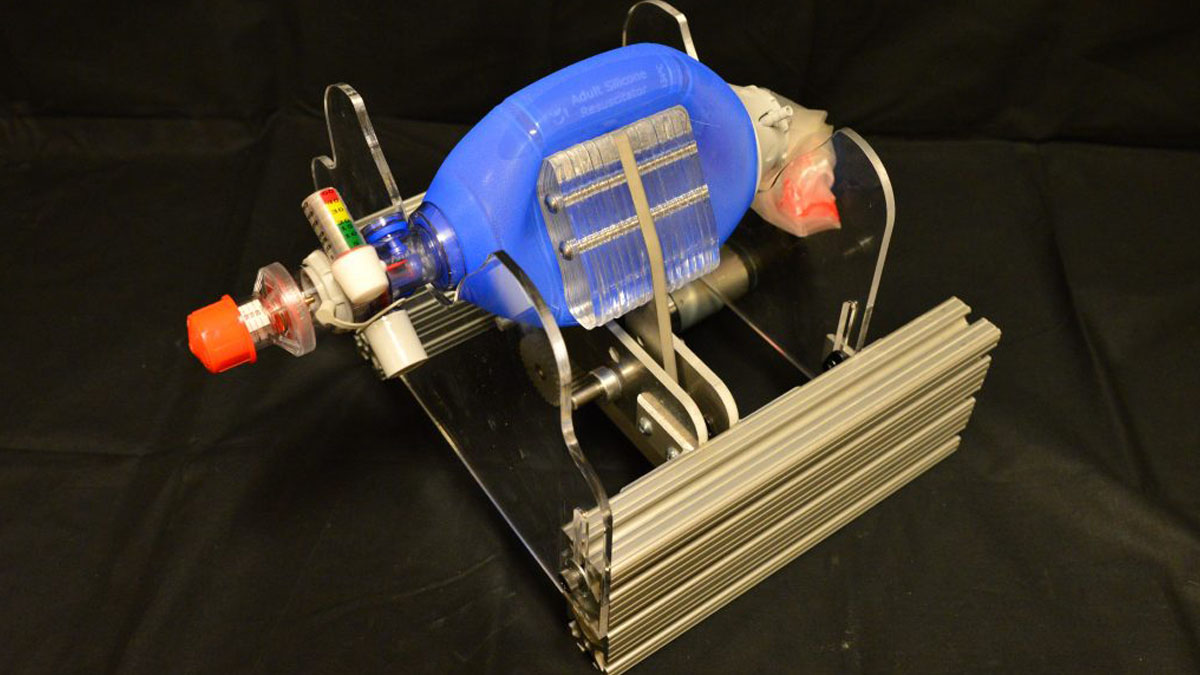
MIT Emergency Ventilator (E-Vent) Project (Open source design)
Read more at: https://e-vent.mit.edu/
The MIT E-Vent project website contains all the technical information needed to build the emergency ventilator, including the ventilation specifications, the clinical considerations, the mechanical design, the contols and electrical design and the DXFs for the custom parts.
Rice University Ventilator
Gtech mechanical ventilator
British home appliances firm Gtech, which specializes in making vacuum cleaners, has made a prototype of a medical ventilator, made largely from off-the-shelf parts, the ventilator runs on compressed air and can be assembled with a simple production line.
Watch the video at: https://youtu.be/DdQg11QgpXg
Key Ventilation Specifications
(From MIT at : https://e-vent.mit.edu/clinical/key-ventilation-specifications/)
Updated 28 March 2020
Note changes to specifications with increased BPM and I:E ratios. Adjusting one of these parameters may influence the other, since at higher BPM, the tidal volume is usually decreased. Consult a clinician.
From the Clinical Guidance this document summarizes the minimum set of requirements for ventilation:
- Patients must be under the management of a trained clinician.
- The minimum controllable parameters in order to ventilate a patient include:
- BPM (breaths per minute): between 8 – 40 BPM
- Tidal Volume (TV) (air volume pushed into lung): between 200 – 800 mL based on patient weight
- I/E Ratio (inspiratory/expiration time ratio): recommended to start around 1:2; best if adjustable between range of 1:1 – 1:4*
- Assist Detection pressure. When a patient tries to inspire, they can cause a dip on teh order of 1 – 5 cm H2O, with respect to PEEP pressure (not necessarily = atmospheric).
- Airway pressure must be monitored
- Maximum pressure should be limited to 40 cm H2O at any time; Plateau pressure should be limited to max 30 cm H2O
- The use of a passive mechanical blow-off valve fixed at 40 cm H2O is strongly recommended
- Clinician require readings of plateau pressure and PEEP (refer to clinical documentation tab)
- PEEP of 5-15 cm H2O required; many patients need 10-15 cmH2O
- Failure conditions must permit conversion to manual clinician override, i.e. if automatic ventilation fails, the conversion to immediate ventilation must be immediate.
- Ventilation on room air is better than no ventilation at all. Blending of oxygen and air gas mixture to adjust FiO2 is not important in an emergency scenario. It is certainly nice to have that ability and can easily be implemented with a oxygen / air gas blender that some hospitals already have.
- Covid-19 can get aerosolized (airborne), so HEPA filtration on the patient’s exhalation is required or between the ventilator unit and the patient (at the end of the endotracheal tube) to protect clinical staff from certain infection. In-line HEPA filters can usually be purchased alongside manual resuscitator bags.
- Heat and moisture exchanger should be used in line with the breathing circuit.
- Failure conditions must result in an alarm.
This is a minimal requirement set for emergency use. Equipment designed for more regular use, even if for emerging markets, will require additional features to be used on a regular basis.
*Range determined based on several COVID-19 patients’ ventilator settings reported from Boston area ICUs
More Reading
(from the University of Florida: https://vam.anest.ufl.edu/reviewventilation.html)
Mechanical and Manual Ventilation Systems
I- Mechanical Ventilation
Function of the Spill Valve (Ventilator Pressure Relief Valve, Exhaust Gas Valve)
Because the APL valve in the breathing system is either closed or isolated during ventilator operation, i.e., mechanical ventilation, each ventilator must contain a spill valve for venting excess gases into the scavenging system. During the expiratory phase of the mechanical ventilation cycle the spill valve vents excess gas; during inspiration it closes. In an upright (not hanging) bellows, the spill valve is weighted such that its opening pressure of 2-4 cm H2O is higher than the pressure required to fill and lift the bellows back to its full position. Therefore, the bellows will fill first and reach the top of its casing before the spill valve will open. The opening pressure of the spill valve causes the "intrinsic PEEP" of 2 -4 cm H2O observed with a standing bellows even if no PEEP is being applied. In a system with no significant leaks, the amount of excess gas vented should approximate the incoming fresh gas flow.
Function of the Proportional Flow Control Valve
Not to be confused with the manually operated flow control valve of the oxygen flowmeter, the proportional flow control valve in the ventilator controls the amount of drive gas (O2 in the case of the Ohmeda 7800 ventilator) that is admitted during mechanical inspiration to the bellows casing to "squeeze" the bellows, and therefore the tidal volume that is delivered to the patient. The exhalation valve is closed during mechancial inspiration and during the inspiratory pause if one is used. The exhalation valve opens during exhalation allowing the drive gas to vent to atmosphere, thus depressurizing the bellows casing to atmospheric pressure.
Different Locations of the APL Valve in Modulus I and II Machines
In the Ohmeda Modulus II machines, the adjustable pressure limiting (APL, aka as "pop-off", valve) is located at a position such that it is in pneumatic conection with the breathing circuit only during manual ventilation (i.e., the selector knob is set to Bag mode). When the selector knob is set to Ventilator mode, the APL valve is no longer part of the circuit. Even if the APL valve is left open, no gas is able to escape out of the APL valve.
In the Modulus I design, the APL valve remains in pneumatic connection with the breathing circuit even when the selector knob is set to Ventilator mode. If the APL valve is accidentally left open during mechanical ventilation, gas will escape to the scavenging system and the patient might be hypoventilated. The delivered tidal volume might be considerably less than that set on the ventilator.
The location of the APL valve in this simulation reflects that of the Modulus II machines.
II- Manual Ventilation
Function of the APL Valve
The APL (Adjustable Pressure Limiting) valve is only used during manual (or spontaneous) ventilation in the Modulus II machines. As its name indicates, the APL valve limits the amount of pressure buildup that can occur during manual ventilation. When the user adjusts the APL valve to trap more gas inside the breathing circuit, a spring inside the APL valve is compressed according to how much the user turns the APL valve. The degree of spring compression exerts a proportional force on a sealing diaphragm in the APL valve. The pressure inside the breathing circuit must generate a force that exceeds the spring compression force for the APL valve to open. As pressure continues to build from the combination of fresh gas flow and manual compression of the breathing bag, the opening pressure of the APL valve will be exceeded and excess gas will be vented to the scavenging system.
With the selector knob set to manual ventilation and the APL valve in half open position, the pressure build-up in the circuit can be seen to overcome the APL opening pressure generated by the compression of the spring inside the APL.
Positions of the APL Valve
The APL valve can either be completely closed (no gas vented), completely open (all gas vented - this makes it impossible to ventilate the patient - no gas buildup is possible and the manual breathing bag stays fully deflated), or any position in between.
Increase in Compliance of the Manual Breathing Bag
With Increasing Bag Volumes
With the APL valve completely closed and the selector knob in the Bag mode, no gas can be vented at all and the breathing bag continues to increase in size. Pressure buildup, however, is quite slow because the compliance of the bag actually increases with increasing bag size. The pressure-volume characteristics of rubber bags are such that the patient is somewhat protected from excessive pressures in the breathing system. Adding volume to a bag causes a negligible rise in the pressure until the nominal capacity is reached. When more volume is added, the pressure rises quickly but then reaches a plateau with the pressures remaining between 30-50 cm H2O. However, non-elastic bags might exceed this limit.
Inflation of the manual bag will initially cause a rapid increase in the inspiratory pressure which can be observed on the inspiratory pressure gauge. After reaching a certain bag volume, the pressures will increase much more slowly.